
 The glistening white tissue that covers the ends of the bones (the joint surface) is both tough and resilient. It is not only important for smooth gliding of the joint, but also to "soften" the impact during loading, like a shock absorber.
The glistening white tissue that covers the ends of the bones (the joint surface) is both tough and resilient. It is not only important for smooth gliding of the joint, but also to "soften" the impact during loading, like a shock absorber.
 This is a technique that stimulates the body to make a repair tissue (fibrocartilage) to fill in the defect in articular cartilage. This repair tissue develops from cells brought to the area with blood from the bone marrow underneath the cartilage. These cells enter through small holes made through the bone by using a small pick to create microfractures.
Compare this to repairing "potholes" in a road to lessen the problem of the hole spreading to the entire road. The "potholes" in the body fill in with a repair cartilage that is made up of biomechanical properties that are not as strong or durable as normal cartilage. It may not last as long as a "normal road", but these techniques are successful in eliminating symptoms in many patients.
This is a technique that stimulates the body to make a repair tissue (fibrocartilage) to fill in the defect in articular cartilage. This repair tissue develops from cells brought to the area with blood from the bone marrow underneath the cartilage. These cells enter through small holes made through the bone by using a small pick to create microfractures.
Compare this to repairing "potholes" in a road to lessen the problem of the hole spreading to the entire road. The "potholes" in the body fill in with a repair cartilage that is made up of biomechanical properties that are not as strong or durable as normal cartilage. It may not last as long as a "normal road", but these techniques are successful in eliminating symptoms in many patients.
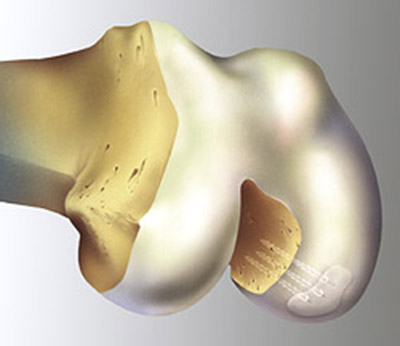
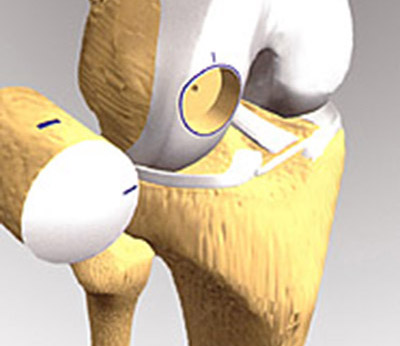
 This bone and cartilage (osteochondral) graft is then transferred to the defect where a receiving hole has been prepared. There is a size limit to the amount of tissue available for "harvesting". The advantage of this technique is the transfer of normal cartilage to the area of injury. The healing is between the bony pieces, much like a broken bone heals. The non-weight-bearing area will eventually heal with scar cartilage much like the micro-fracture technique.
This bone and cartilage (osteochondral) graft is then transferred to the defect where a receiving hole has been prepared. There is a size limit to the amount of tissue available for "harvesting". The advantage of this technique is the transfer of normal cartilage to the area of injury. The healing is between the bony pieces, much like a broken bone heals. The non-weight-bearing area will eventually heal with scar cartilage much like the micro-fracture technique.
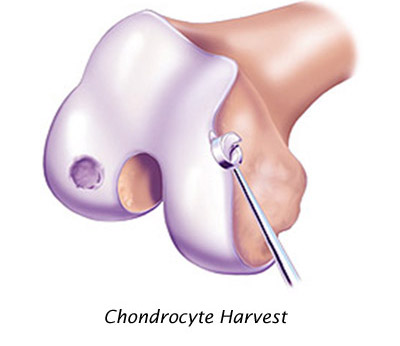
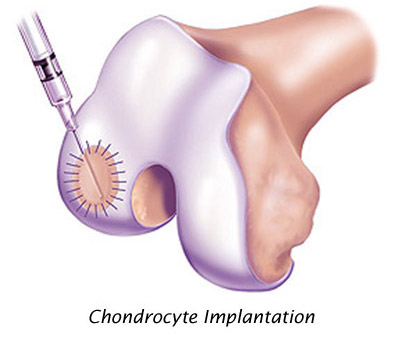 These autologous (your own) cultured chondrocyte cells are then implanted in the knee in a second surgical procedure, under a patch that is sewn to the neighboring cartilage. The chondrocyte cells must create the supporting structure (matrix) over several months to restore the articular surface.
These autologous (your own) cultured chondrocyte cells are then implanted in the knee in a second surgical procedure, under a patch that is sewn to the neighboring cartilage. The chondrocyte cells must create the supporting structure (matrix) over several months to restore the articular surface.
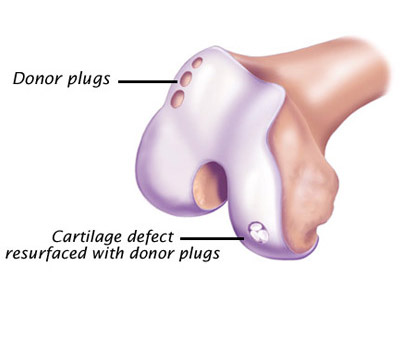
 For larger defects of both bone and cartilage loss, Dr. Mullen may custom fit an implant of freshly donated cadaver cartilage and bone. This implant is press fit into the prepared articular cartilage-bone defect. Specialized instruments provide for the precise matching of the donated tissue. This transplant may allow restoration of the joint surface.
For larger defects of both bone and cartilage loss, Dr. Mullen may custom fit an implant of freshly donated cadaver cartilage and bone. This implant is press fit into the prepared articular cartilage-bone defect. Specialized instruments provide for the precise matching of the donated tissue. This transplant may allow restoration of the joint surface.
